Burn Reconstruction
Burns caused by heat, chemicals and fires can result in the most traumatic types of scaring. The severity of burns is classified as first, second and third degree burn. This designation is based on the dept of damage to the outer and deeper layers of the epidermis (skin) and dermis (inner skin) tissue.
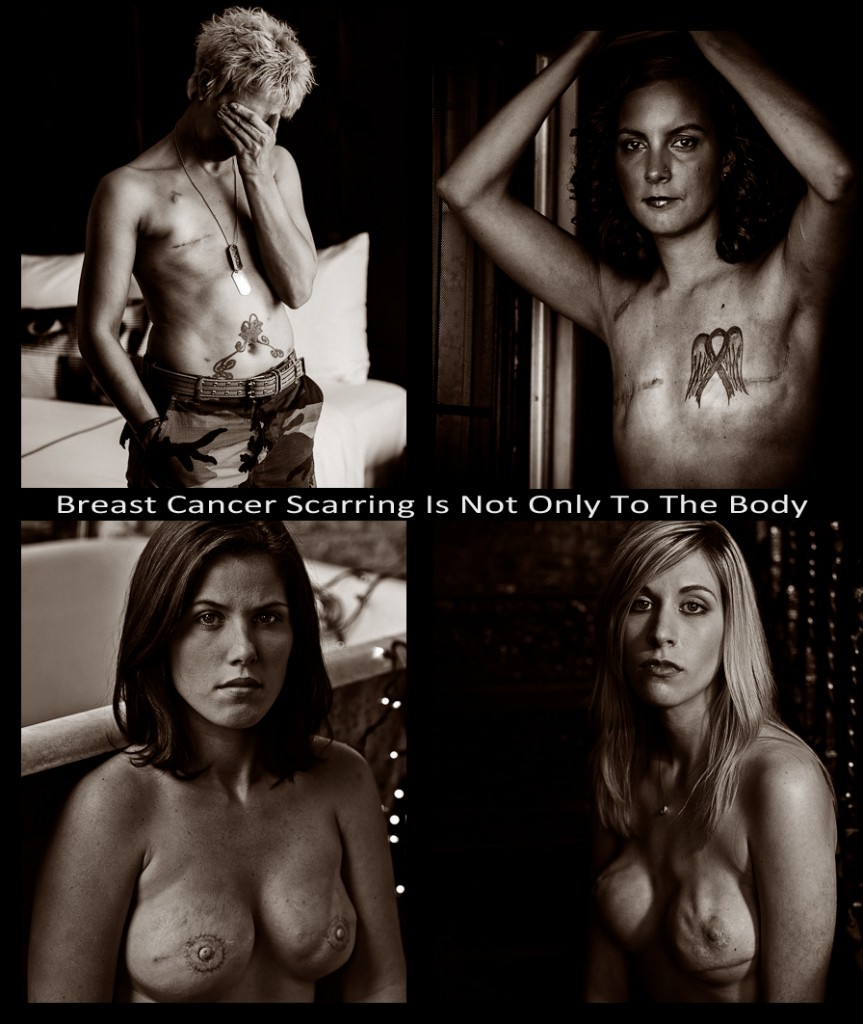
Burns can leave patients with severe physical disfigurements.
The emotional trauma can often exceed the physical trauma as self image is an integral part of an individual’s self esteem. Scar revision surgery for all types of scars is often elected to positively affect the patient’s emotional well being.
Burn treatments usually involve skin grafting and cosmetic reconstruction, and may be performed in an emergency facility or later on. These treatments also focus on restoring function to the burned skin to reduce the risk of complications such as loss of mobility or a loss of one of the senses.
Acute Burn Care
Any type of burn on the skin requires immediate medical attention to stabilize the patient, clean the wound and reduce the risk of complications such as infection, scarring, breathing problems and limited bone and joint mobility. Initial burn care focuses on assessing and treating the initial burn symptoms, prevents infections and other potential further risks. Additional treatment may be required at a later time for skin reconstruction. It is also important for patients to remain hydrated after a burn, so fluids may be administered intravenously to prevent dehydration.
Comprehensive burn care that includes an evaluation of:
• the burn and any related conditions
• thorough wound care
• proper dressing
• pain mitigation through medications
• emergency surgery as may be required.
Burn Scars
Most burns will usually leave a scar,The appearance of the scar depends on the size, location and severity of the burn. Scars usually become less noticeable over time, however when they scar is obvious patients seek reconstructive treatment to improve their appearance of scars that are physically unattractive or disfiguring. Reconstructive procedures are most often performed after the burn has fully healed, which may be nine months to a year after the original injury.
Scar reconstruction is usually performed through an outpatient surgical procedure that may involve skin and tissue grafts, skin flaps or injectable fillers to restore a more natural appearance, while also correcting any functional problems caused by the scar and improving the patient’s self-confidence as well.
Contractures
A contracture is a complication of burn scarring that involves a tightening and thickening of the burn scar that in turn restricts movement of the affected area. It is important for patients to take precautions to prevent contractures from occurring, by exercising, wearing a splint and continuing to promote everyday activities that require movement.
Treatment for contracture scars often involves surgery to release the contracture and restore normal movement to the skin. A skin flap or graft may be used to restore the appearance of the skin in the treated area, while also improving movement and flexibility that may have been affected by the contracture. Physical therapy will often be needed after surgery to stretch the joints and restore movement and function.