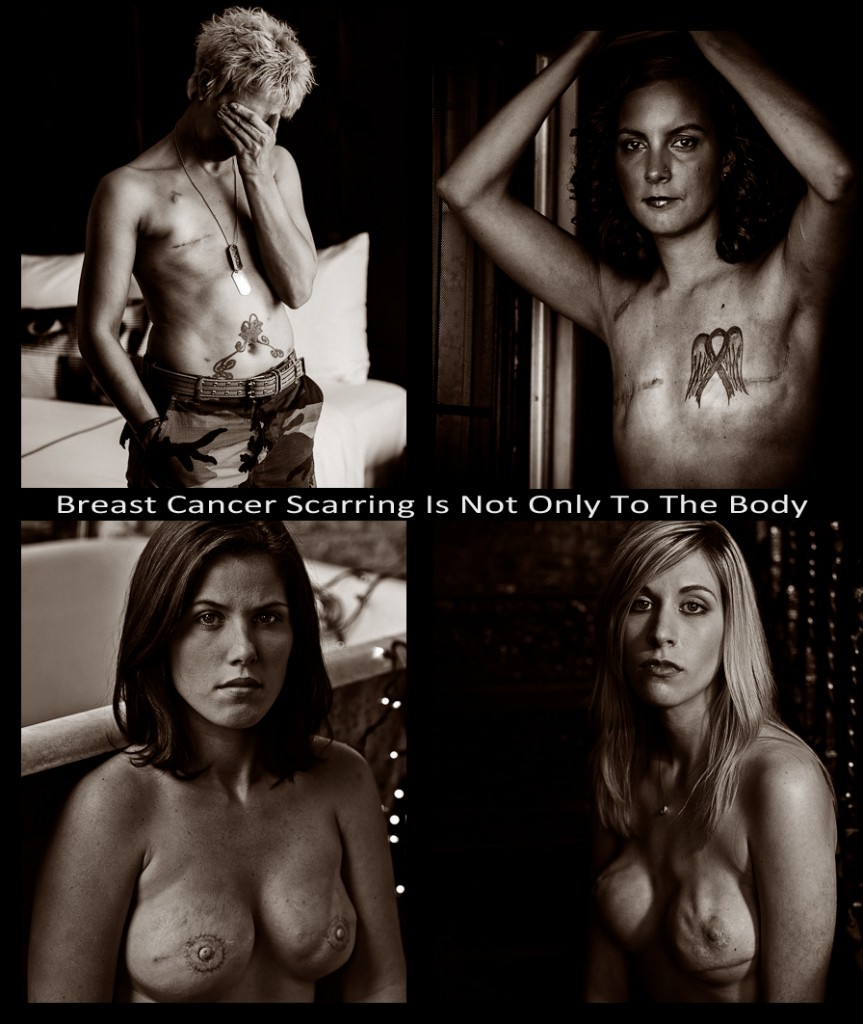
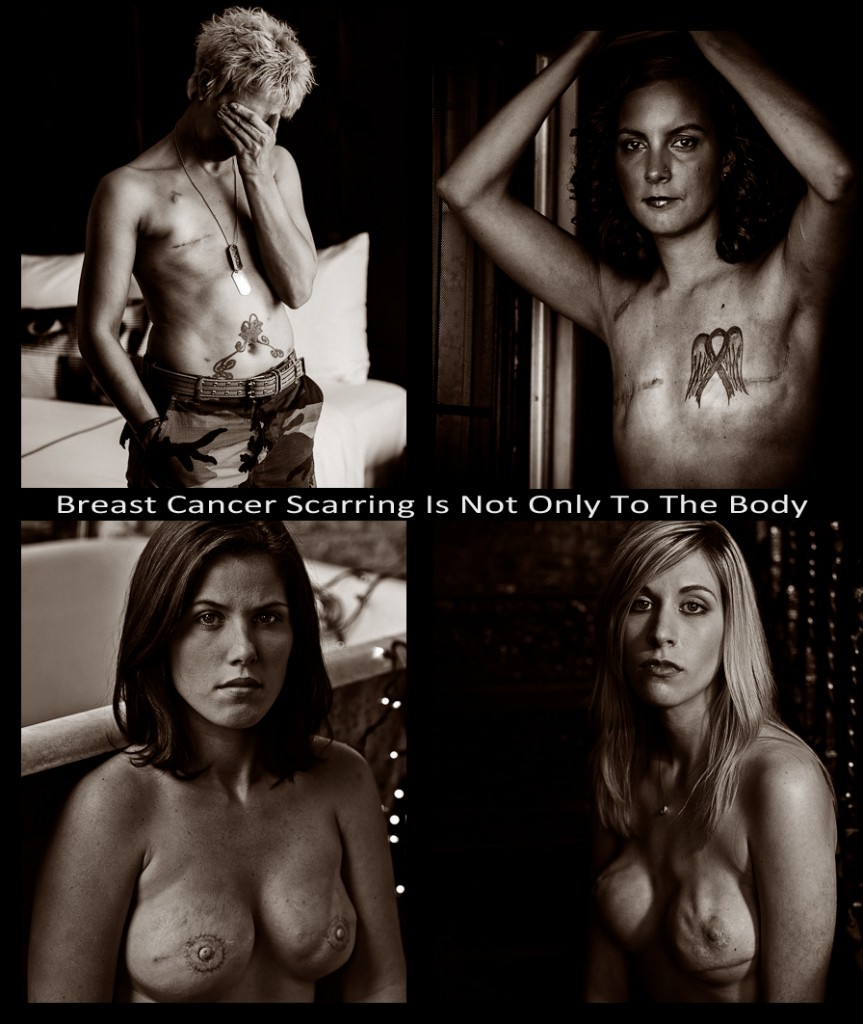
Scarring and Breast Cancer
Healing and Coping with Physical and Emotional Scars
Breast cancer is often treated by minor or major surgical intervention; from a lumpectomy to radical mastectomy life changing surgery takes place. This means that the treatment of breast cancer surgery that unavoidably leaves scarring as part of the process. The concern for loss of life is for many women often underscore by the fear of disfigurement and loss of feminine ideal and beauty. However this is not inevitable.
The journey to healing from breast cancer surgery always leaves the challenge of mitigation scarring from the minor to major depending upon the surgical treatment required to restore the patient’s health. Even radiation therapy can leave lasting marks. These scars can range from localized, temporary burns that resemble sunburn or a hardened, rigid-type known as radiation fibrosis. Chemotherapy can potentially leave some scarring. The chemotherapeutic medicine is often delivered through an intravenous line or catheter, and since these catheters are inserted during minor surgical procedures that pierce the skin. In some cases a patient’s ability to heal has seriously been compromised; these minor procedures can cause scarring at the site. In extreme instances sites may have to be rotated because of the patient’s inability to heal well and the subsequent scarring.
Factors that Affect Scarring
The breadth and or amount of scarring from breast cancer treatments depends on several factors:
• the type of surgery performed
• each patient’s individual capacity to form scar tissue.
•
Lumpectomy & Mastectomy Scarring
Sixty percent of patients prefer for lumpectomies, surgery that spares the breast and much of the surrounding tissue while removing the cancerous tumor or cells. Still scarring can be a problem. These surgeries range from the removal of a very small amount of breast tissue for testing; to having a full quarter of the breast taken to eradicate the cancer. The result is quite often an asymmetry in the shape of the breast that is emotionally disconcerting to the patient. This feeling is part of the emotional despair experienced by the forty percent of patients who undergo a modified radical mastectomy or the radical surgical removal of the entire breast. These invasive surgical procedures result in a long, slit-like scar that runs from the breastbone to up under the pit of the arm.
For both the lumpectomy and the mastectomy, breast reconstruction is optional, but one of the ways to achieve this actually results in at least one more scar. A flap of tissue can be taken from the women’s abdomen or other area of the body, depending on the amount needed to restore the form of the breast, this results in additional scarring at the site from where the tissue was taken from.
Scars, Body Image, and Intimacy
“Some women choose mastectomy with reconstruction, because they feel there will be a better cosmetic outcome,” says Debbie Saslow, PhD, director of breast and gynecologic cancer at the American Cancer Society in Atlanta. “Some women have a really strong reaction to the scarring – it affects their body image and their sex lives – and other women can almost ignore it.”
The overt presence of scars that are difficult to disguise when a mastectomy patients disrobe can be troublesome for the patient. Many patients who initially decide against breast reconstruction opt for it ater which makes for a more difficult surgery. Patients are not only self conscious about the scars; they fear having to explain them in intimate relationships. This underscores the importance of having a fully holistic team prior to surgery. A consult with counselors and plastic surgeons should be utilized to address the concerns and fears prior to surgery. Discussing with other breast cancer patients who have undergone the surgery is helpful. Those who have and have not opted for breast reconstruction is advisable.
Healing and Reducing Scars
Some of the best ways to limit scarring are:
• by preventing infection immediately after surgery
• lightly stretching and massing the scar area daily during the first year, when most healing occurs
• medical consult with surgeon specializing in scar revision
• ensuring proper surgical site drainage which is inevitable
• keeping the wound clean
• following physicians orders in bandaging the wound
• transverse friction massage by a therapist
The implications of scarring aren’t only in appearance. There can also be pain associated with tightness and pulling. This can be moderate to severe in patients. Various professional modalities and therapies can be used to guide and assist the patient in their wound healing. Some are deep and soft-tissue massage, physical therapy if the muscular structures of the chest and shoulders have been involved to any degree. Alternative therapies such as yoga, which involves deep breathing and full-body stretches, as well as, acupuncture can be used to assist in the recovery of patients who have undergone surgery from breast cancer.