When your hair curls around and can’t grow out of the skin it is referred to as an ingrown hair. This problem is commonly mistaken for pimples. Ingrown hair is known to be found on the cheeks and neck for men, especially after shaving. Women in most cases find ingrown hair on their legs and sensitive shaving areas. Those who have curly hair are more prone to getting ingrown hairs, especially because their hair can easily be curled underneath the skin preventing it from growing out properly.
 Just like what is seen with pimples, when one has an ingrown hair, it produces a small raised red bump. That bump will be itchy and many times might be sore to the touch. Treatment for ingrown hair may not be necessary at all times because ingrown hair sometimes tends to go away on its own. However, if the ingrown hair does not go away, it is best to treat it as it may leave a dark spot or scar on your skin. If an ingrown hair becomes infected, a doctor’s visit is necessary where they can safely use a needle to release the hair.
Just like what is seen with pimples, when one has an ingrown hair, it produces a small raised red bump. That bump will be itchy and many times might be sore to the touch. Treatment for ingrown hair may not be necessary at all times because ingrown hair sometimes tends to go away on its own. However, if the ingrown hair does not go away, it is best to treat it as it may leave a dark spot or scar on your skin. If an ingrown hair becomes infected, a doctor’s visit is necessary where they can safely use a needle to release the hair.
If you have scarring from an ingrown hair, it is best to see a dermatologist so they can observe the scarring and recommend treatment options for you. Some treatment options may consist of using a bleaching cream, laser treatment, microdermabrasion, or chemical peels.

 Keratosis pilaris is not harmful, so medical treatment is not necessary. However, scarring may occur as a result of this condition, so it is recommended to exfoliate with a mild soap and moisturize skin at least twice a day. Over-the-counter creams and lotions are what most people use to treat this condition. The effectiveness of these creams is very limited. There have been a few cases that it was treated by laser therapy, however research is still being done to find out the best treatment for this condition.
Keratosis pilaris is not harmful, so medical treatment is not necessary. However, scarring may occur as a result of this condition, so it is recommended to exfoliate with a mild soap and moisturize skin at least twice a day. Over-the-counter creams and lotions are what most people use to treat this condition. The effectiveness of these creams is very limited. There have been a few cases that it was treated by laser therapy, however research is still being done to find out the best treatment for this condition. 

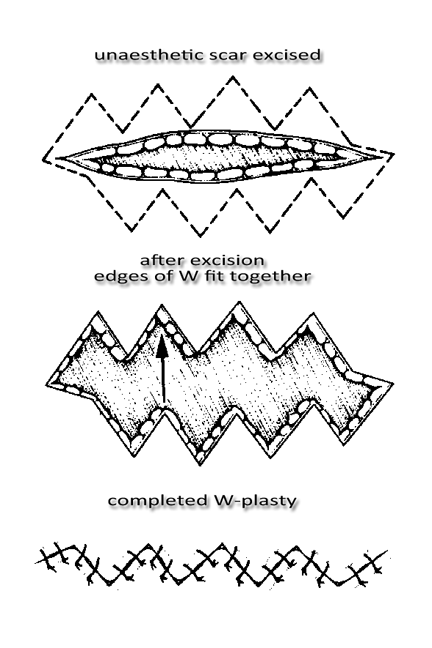
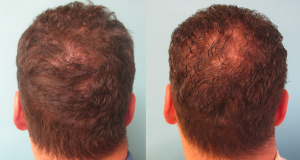
 Scarring is the result of tissue fibers replacing normal skin after a trauma. Scarring can result from surgery, burns, open wounds, or any other abrasion of the skin. Scars are caused when the deep thick layer of skin, also known as the dermis, is damaged. Once trauma occurs, the body forms a collagen fiber which aids in the healing process of the wound and causes a scar. Because the tissue is a different consistency and quality the scar becomes visible.
Scarring is the result of tissue fibers replacing normal skin after a trauma. Scarring can result from surgery, burns, open wounds, or any other abrasion of the skin. Scars are caused when the deep thick layer of skin, also known as the dermis, is damaged. Once trauma occurs, the body forms a collagen fiber which aids in the healing process of the wound and causes a scar. Because the tissue is a different consistency and quality the scar becomes visible.